Abstract
Whipple’s Disease is a rare multisystemic disorder caused by the bacterium Tropheryma whipplei, which can lead to significant central nervous system involvement. This review synthesizes current knowledge on the neuropathogenesis, clinical manifestations, diagnostic approaches, and therapeutic interventions for Whipple’s Disease, emphasizing its neurological implications.
Introduction
Whipple’s Disease is an infrequent systemic illness traditionally characterized by gastrointestinal manifestations but increasingly recognized for its neurological involvement. The disease is attributable to infection by the actinomycete Tropheryma whipplei. While the gastrointestinal tract is the primary site of infection, the bacterium can disseminate, leading to a range of clinical symptoms, with the central nervous system being a critical site of secondary involvement. CNS-infiltrating Whipple’s Disease often results in a complex array of neurological and psychiatric symptoms that can precede, follow, or occur independently of intestinal involvement.
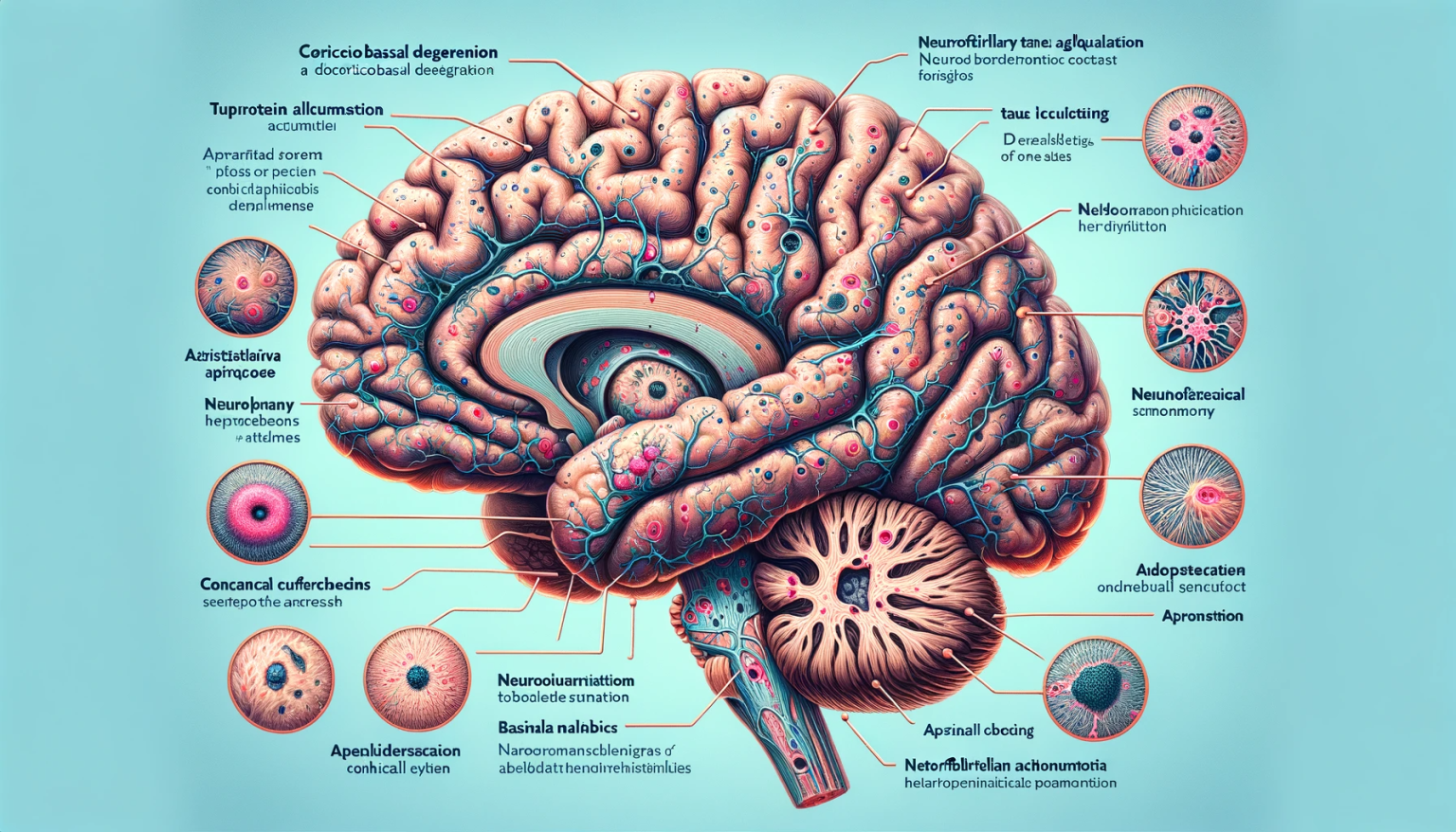
Neuropathogenesis
The pathogenic mechanisms by which T. whipplei affects the CNS remain under investigation. The bacterium demonstrates a remarkable ability to evade the immune system, resulting in chronic infection and granulomatous inflammation. In susceptible individuals, the organism breaches the intestinal barrier, disseminates through the bloodstream, and crosses the blood-brain barrier, leading to a range of neuropathological changes. These include microglial activation, neuronal loss, and the formation of characteristic periodic acid-Schiff (PAS)-positive macrophages within the CNS parenchyma.
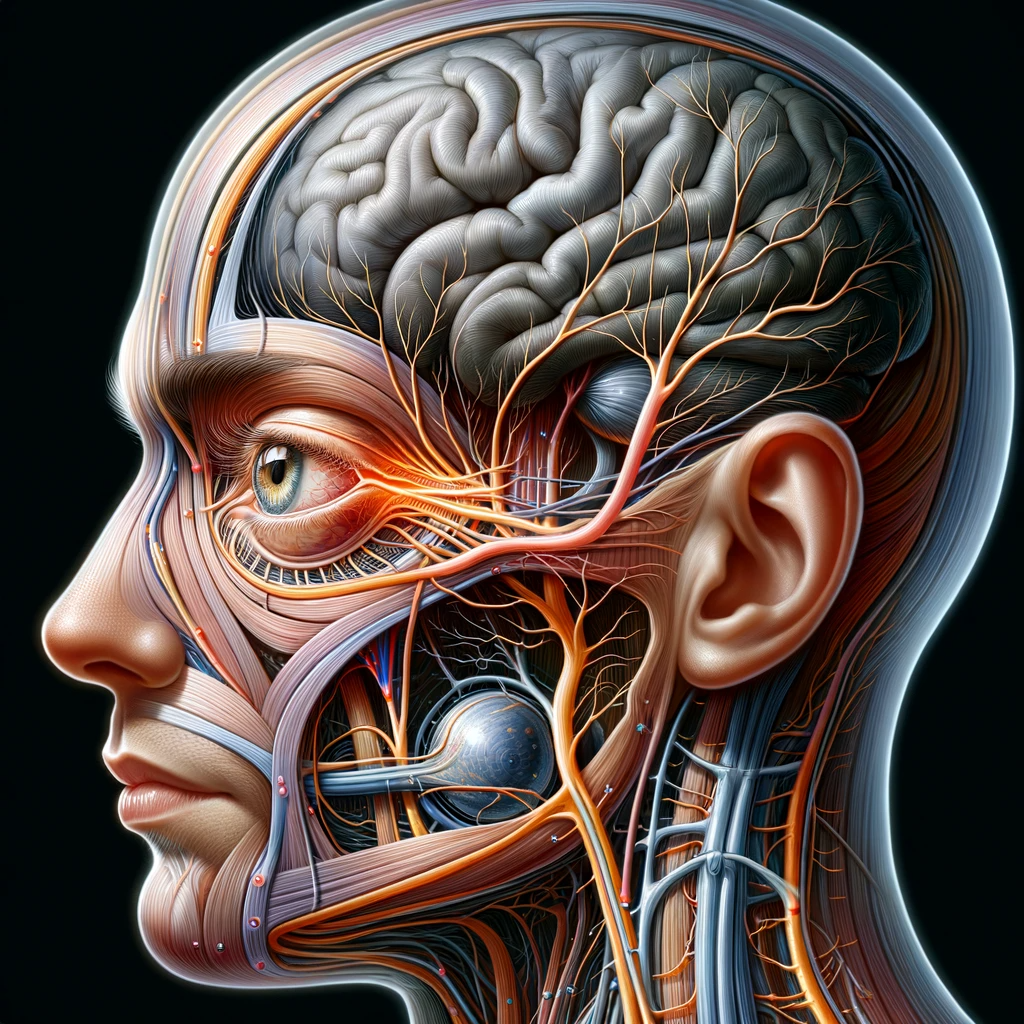
Clinical Presentation
Neurological manifestations of Whipple’s Disease are diverse and can often mimic other neurodegenerative disorders. Patients may present with cognitive decline, memory impairment, ataxia, oculomasticatory myorhythmia, and supranuclear ophthalmoplegia. Psychiatric symptoms such as mood swings, personality changes, and delirium are also commonly reported. The variability in the presentation often leads to diagnostic delays and challenges.
Diagnostic Approach
The diagnosis of CNS-involving Whipple’s Disease is multifaceted, integrating clinical, radiological, and laboratory findings. Magnetic resonance imaging (MRI) may reveal nonspecific white matter changes, while cerebrospinal fluid (CSF) analysis can detect pleocytosis and elevated protein levels. Definitive diagnosis relies on the identification of T. whipplei DNA in the CSF or brain tissue via polymerase chain reaction (PCR), supported by PAS staining of affected tissues showing diastase-resistant granules.
Therapeutic Interventions
Treatment of CNS-involving Whipple’s Disease requires an aggressive and prolonged course of antibiotics to penetrate the blood-brain barrier effectively. Regimens typically include a combination of intravenous ceftriaxone or penicillin G, followed by oral trimethoprim-sulfamethoxazole for one to two years. Clinical response to therapy is monitored through serial neurological examinations and repeated CSF analysis. The management of refractory cases may necessitate alternative antibiotic therapies or the addition of immunomodulatory agents.
Conclusion
Whipple’s Disease with CNS involvement is a rare yet severe condition that necessitates a high index of suspicion for timely diagnosis and intervention. As clinical manifestations can be protean and nonspecific, a combination of advanced diagnostic techniques and empiric therapeutic trials is often essential. Interdisciplinary collaboration across gastroenterology, neurology, infectious disease, and pathology specialties is critical for optimal patient outcomes.