 Abstract
Abstract
Striatonigral Degeneration (SND) is a progressive neurological disorder that falls under the umbrella of multiple system atrophy. This extensive review aims to elucidate the pathophysiological mechanisms, clinical features, diagnostic challenges, and current therapeutic strategies associated with SND.
Introduction
Striatonigral Degeneration, a subtype of multiple system atrophy (MSA), primarily affects the striatonigral pathway in the brain. It is characterized by a combination of parkinsonian symptoms and atypical features, often leading to misdiagnosis in early stages. Understanding SND is essential for accurate diagnosis and management, given its progressive and debilitating nature.
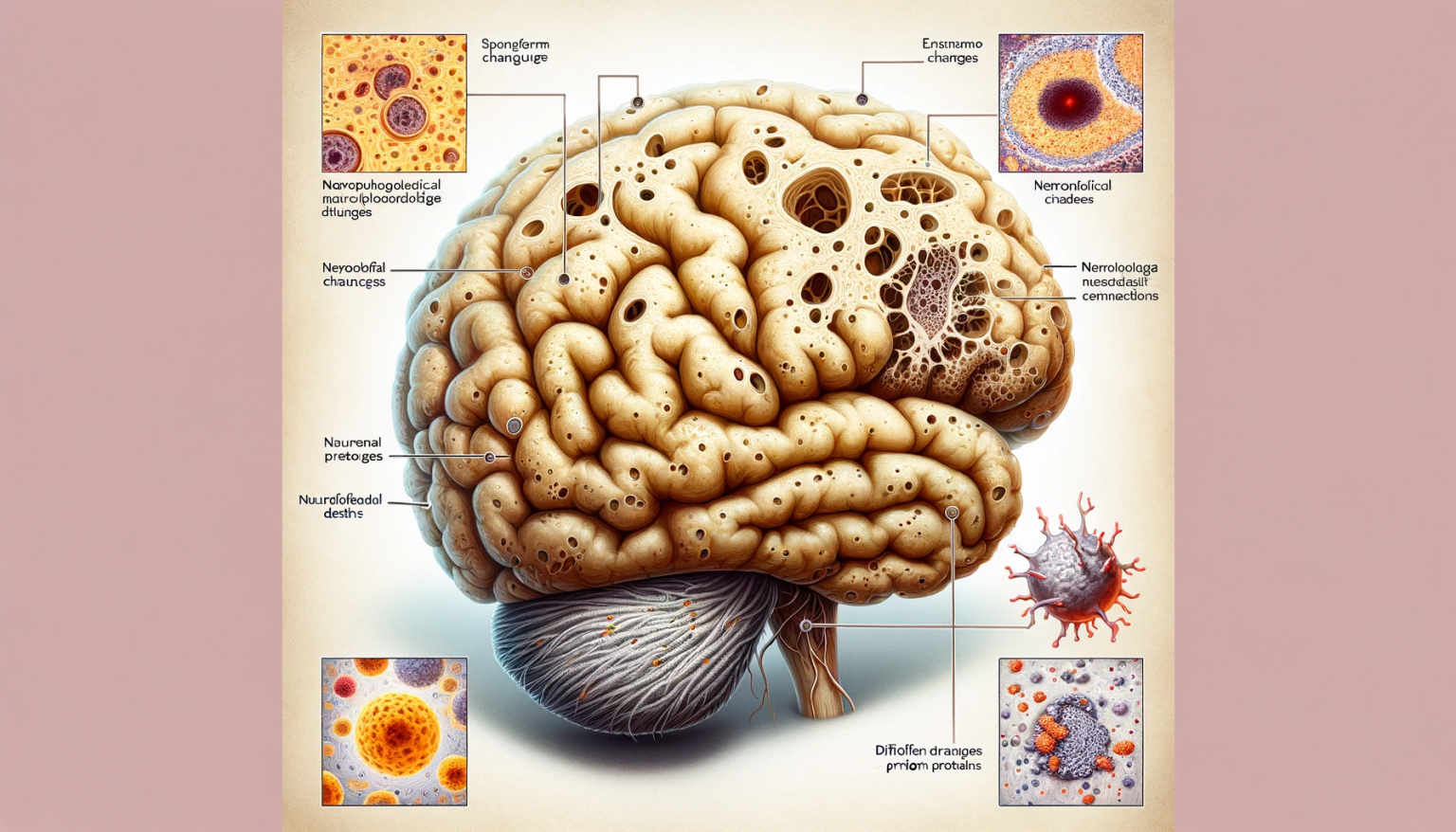
Pathophysiology
SND involves the progressive degeneration of the striatum and substantia nigra, two critical components of the basal ganglia system involved in movement control. The hallmark of the disease is the accumulation of alpha-synuclein protein in glial cytoplasmic inclusions within these regions, leading to neuronal loss and dysfunction. This pathology is thought to underlie the motor symptoms observed in SND.
Clinical Presentation
Patients with SND typically exhibit parkinsonian features such as bradykinesia, rigidity, and tremor. However, unlike Parkinson’s disease, SND presents with poor response to levodopa, a key differentiating factor. Other symptoms include postural instability, speech and swallowing difficulties, and sometimes autonomic dysfunction. Cognitive impairment and emotional disturbances may also occur as the disease progresses.
Diagnostic Approach
Diagnosis of SND is primarily clinical, supplemented by neuroimaging techniques like MRI, which may show atrophy in the affected regions. However, definitive diagnosis often requires neuropathological examination, with the presence of glial cytoplasmic inclusions being a key diagnostic feature. Differential diagnosis includes Parkinson’s disease, corticobasal degeneration, and other forms of atypical parkinsonism.
Therapeutic Management
Treatment of SND is mainly symptomatic and supportive. Dopaminergic therapies, commonly used in Parkinson’s disease, have limited efficacy in SND. Physical therapy and occupational therapy are crucial in managing motor symptoms and maintaining functional independence. Autonomic symptoms, such as orthostatic hypotension, require specific management strategies. Research into neuroprotective strategies and disease-modifying treatments is ongoing but has yet to yield definitive results.
Prognosis and Future Directions
The prognosis of SND is generally poor, with a progressive decline leading to significant disability and eventual mortality. Research efforts are focused on understanding the molecular mechanisms underlying alpha-synuclein accumulation and identifying potential therapeutic targets to modify disease progression.
Conclusion
Striatonigral Degeneration presents significant challenges in neurology, particularly in terms of diagnosis and management. A deeper understanding of its pathophysiology and clinical spectrum is essential for developing more effective treatments and improving the quality of life for affected individuals.