 Abstract: Meningitis, an acute inflammation of the meninges, can lead to various long-term neurological complications, despite successful initial treatment. This review explores the spectrum of post-meningitis sequelae, emphasizing the underlying pathophysiological mechanisms and the clinical management of these persistent symptoms.
Abstract: Meningitis, an acute inflammation of the meninges, can lead to various long-term neurological complications, despite successful initial treatment. This review explores the spectrum of post-meningitis sequelae, emphasizing the underlying pathophysiological mechanisms and the clinical management of these persistent symptoms.
Introduction: Meningitis, caused by viral, bacterial, or other microbial agents, is a serious medical condition characterized by the inflammation of the meningeal coverings of the brain and spinal cord. While advancements in antimicrobial therapies have reduced mortality rates, survivors often face a range of post-infectious sequelae, whose intensity varies depending on the etiology of meningitis, the age of the patient, and the promptness and effectiveness of initial treatment.
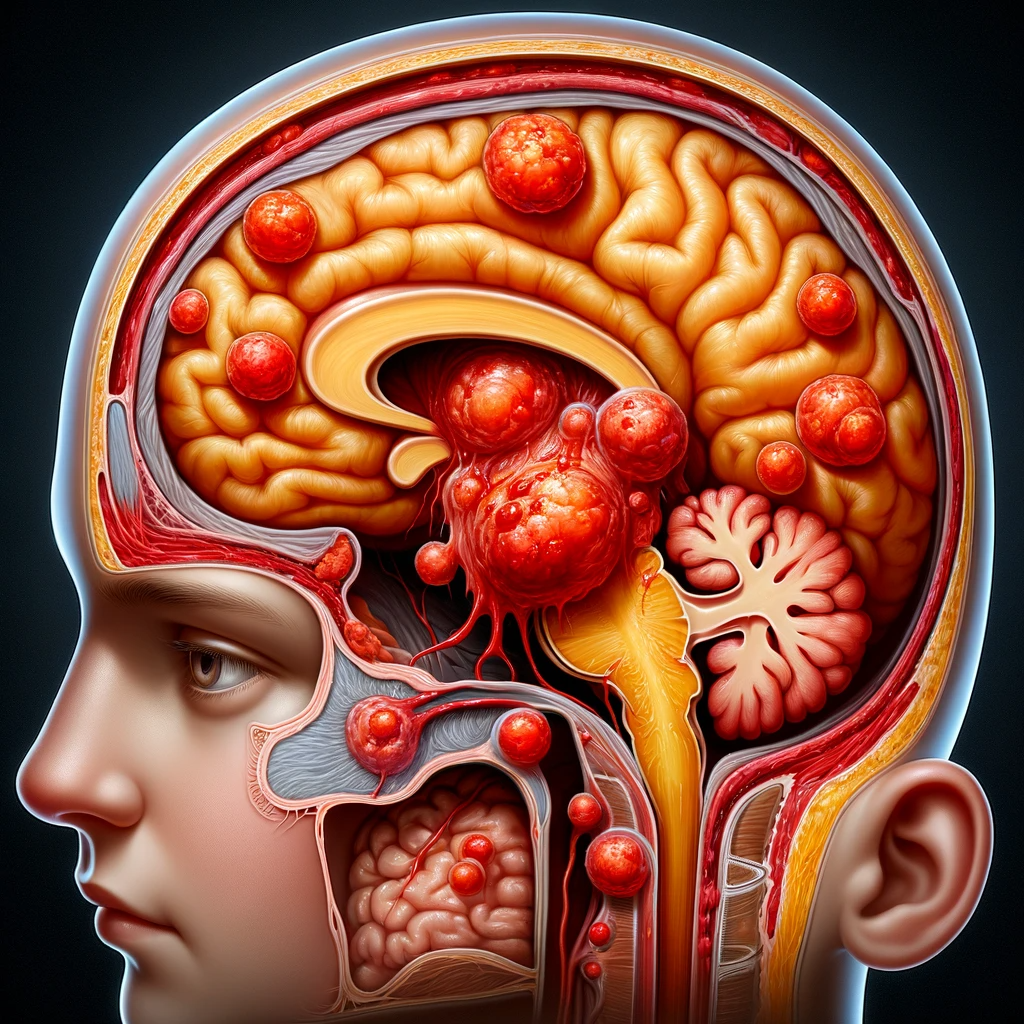
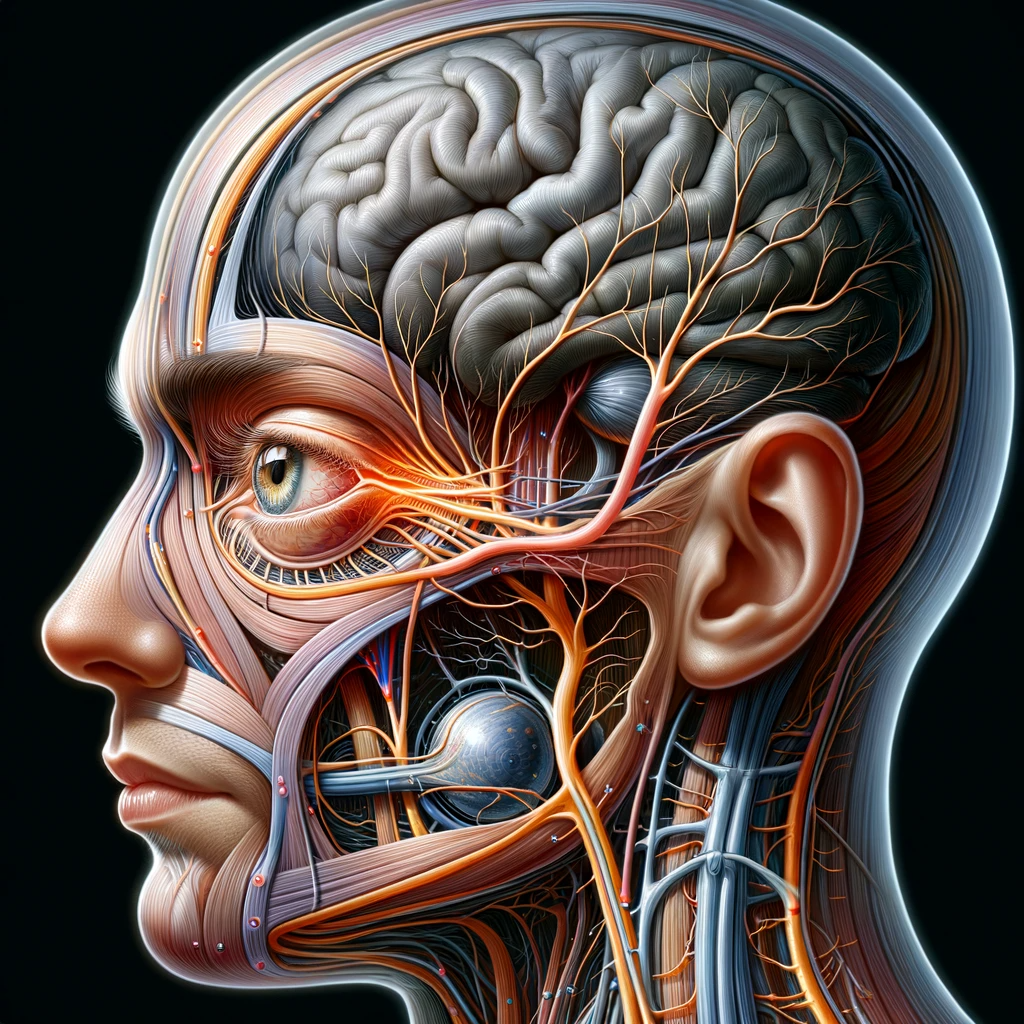
Pathophysiology: The mechanisms leading to post-meningitis damage are multifactorial. Bacterial meningitis, in particular, can lead to a robust immune response, causing increased intracranial pressure, cerebral edema, and ischemia. The resultant neuronal damage can be permanent, leading to various neurological deficits. Viral meningitis, while generally less severe, can also result in lasting neurological effects.
Neurological Complications: Post-meningitis sequelae can range from mild cognitive impairments to severe neurological deficits. Common complications include:
- Sensorineural Hearing Loss: This is one of the most common sequelae, particularly in bacterial meningitis, attributed to cochlear nerve damage.
- Cognitive Deficits: These may include memory impairment, reduced attention span, and executive dysfunction.
- Motor Deficits: Patients may experience muscle weakness, spasticity, and coordination issues.
- Seizures and Epilepsy: Meningitis can increase the risk of seizure disorders due to neuronal damage and scarring.
- Hydrocephalus: Increased cerebrospinal fluid (CSF) production or impaired absorption can lead to hydrocephalus.
- Psychiatric Disorders: Anxiety, depression, and Post-traumatic Stress Disorder (PTSD) are reported in some survivors.
Clinical Management: Managing post-meningitis sequelae involves a multidisciplinary approach:
- Rehabilitative Services: Physical, occupational, and speech therapy are critical for functional recovery.
- Neurocognitive Assessment and Support: Neuropsychological evaluations and tailored cognitive rehabilitation can help address cognitive impairments.
- Audiological Evaluation and Management: Regular hearing assessments and interventions, such as hearing aids or cochlear implants, are essential for those with hearing loss.
- Antiepileptic Therapy: In cases of seizures, appropriate antiepileptic drugs are prescribed.
- Neuropsychiatric Support: Counseling and psychiatric medications can be beneficial for mental health issues.
Conclusion: The post-meningitis landscape is complex, with a diverse array of potential long-term effects. Early recognition and comprehensive management of these sequelae are essential for improving the quality of life of survivors.