Abstract
Neuronal Ceroid Lipofuscinoses (NCLs) represent a group of rare, inherited, progressive neurodegenerative disorders primarily affecting children. This extensive review delves into the molecular genetics, clinical manifestations, diagnostic methodologies, and current therapeutic approaches in NCLs.
Introduction
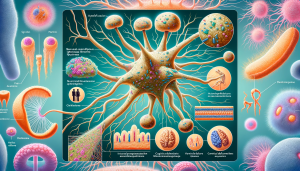
Neuronal Ceroid Lipofuscinoses, commonly referred to as Batten disease, encompass a group of lysosomal storage disorders. They are characterized by the accumulation of lipofuscins within neurons, leading to progressive neurological decline. NCLs are clinically and genetically heterogeneous, with various forms classified based on age of onset and specific genetic mutations.
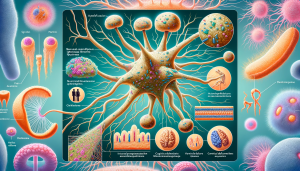
Molecular Pathogenesis
The underlying cause of NCLs is mutations in at least 13 different genes (CLN1-CLN8, CLN10-CLN14). These genes encode proteins involved in lysosomal function and cellular waste processing. Mutations result in the accumulation of autofluorescent lipopigments, primarily subunit c of mitochondrial ATP synthase and saposins. This accumulation disrupts cellular function, leading to neuron death and brain atrophy.
Clinical Presentation
NCLs are categorized by age of onset: infantile (INCL), late infantile (LINCL), juvenile (JNCL), and adult-onset. Common initial symptoms include vision loss, cognitive decline, and seizures. As NCLs progress, patients experience motor deterioration, speech impairment, and behavioral changes. Each subtype has distinct clinical features and progression rates.
Diagnostic Approach
Diagnosis involves clinical assessment, visual and neurological examination, and confirmation through genetic testing. Electron microscopy of skin or other tissue biopsies may reveal characteristic lipopigment patterns. Enzyme assays and imaging studies, such as MRI, contribute to the diagnostic process. Molecular genetic testing identifies specific gene mutations, aiding in definitive diagnosis and genetic counseling.
Therapeutic Management
Currently, there is no cure for NCLs, and treatment focuses on symptom management and supportive care. Antiepileptic drugs control seizures, while physical, occupational, and speech therapies help maintain function. Nutritional support and management of psychiatric symptoms are also critical. Emerging therapies, including gene therapy and enzyme replacement therapy, are under investigation.
Prognosis and Future Directions
The prognosis for NCLs varies, with most forms leading to premature death. Research is ongoing to understand the molecular mechanisms underlying NCLs and to develop targeted therapies. Clinical trials for gene therapy and other novel interventions hold promise for altering the disease course.
Conclusion
Neuronal Ceroid Lipofuscinoses present a complex challenge in pediatric neurology and genetics. A comprehensive understanding of their molecular basis, clinical diversity, and management is crucial for improving patient outcomes and advancing towards effective treatments.