Abstract: Diabetes Mellitus (DM), a systemic metabolic disorder, is increasingly recognized for its diverse and profound effects on the nervous system. This article delineates the neurological consequences of DM, encompassing both central and peripheral nervous system complications, their pathophysiological underpinnings, clinical manifestations, diagnostic approaches, and management strategies.

Introduction: The global prevalence of DM and its chronic nature have profound implications for neurological health. Hyperglycemia and insulin resistance, hallmarks of DM, play pivotal roles in the development of diabetic neuropathies and other neurologic sequelae.
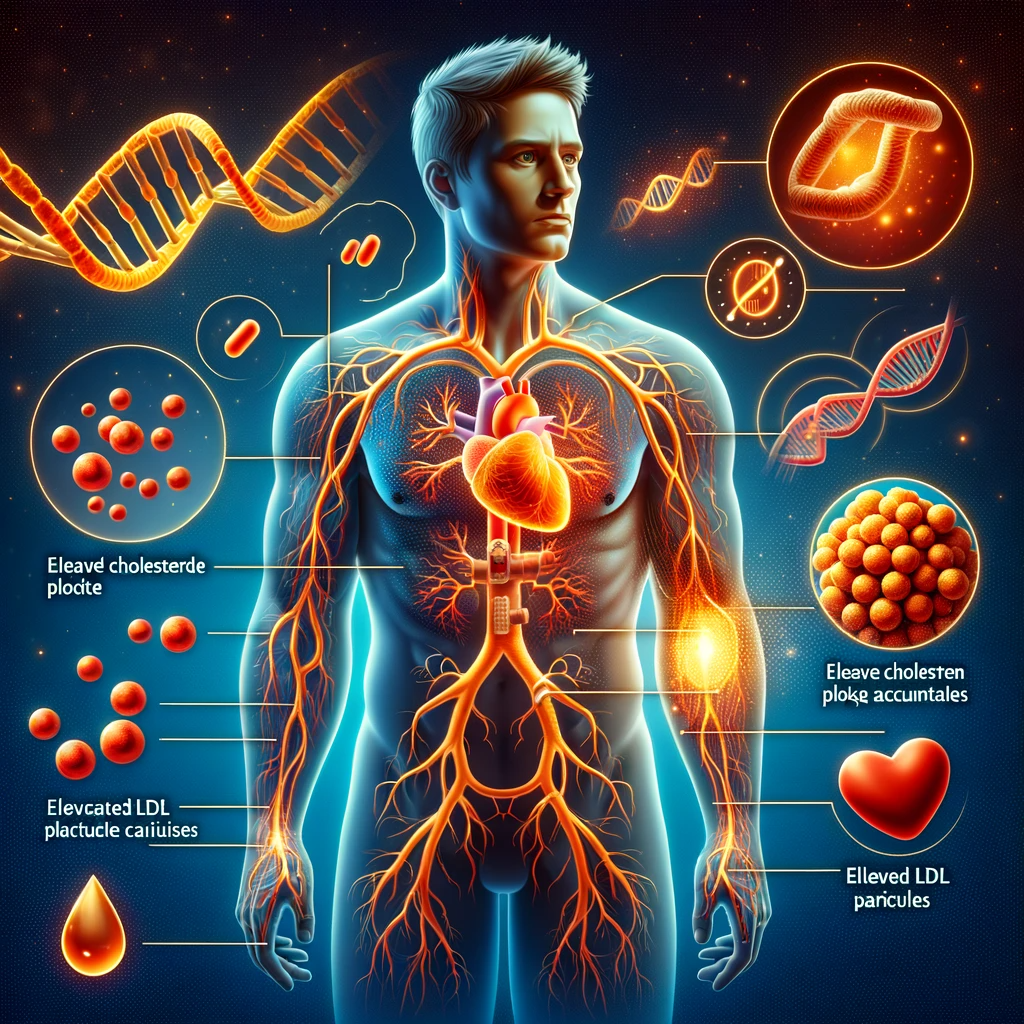
Pathophysiology: The neurological complications in DM are attributed to:
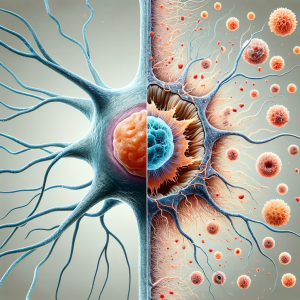
- Metabolic Disruptions: Chronic hyperglycemia leads to glycation end products, oxidative stress, and inflammatory pathways activation.
- Vascular Changes: Microvascular and macrovascular complications compromise blood supply to neural tissues.
- Neuronal and Glial Cell Alterations: Direct glucose toxicity, along with altered insulin signaling, affects neuronal and glial cell functions.
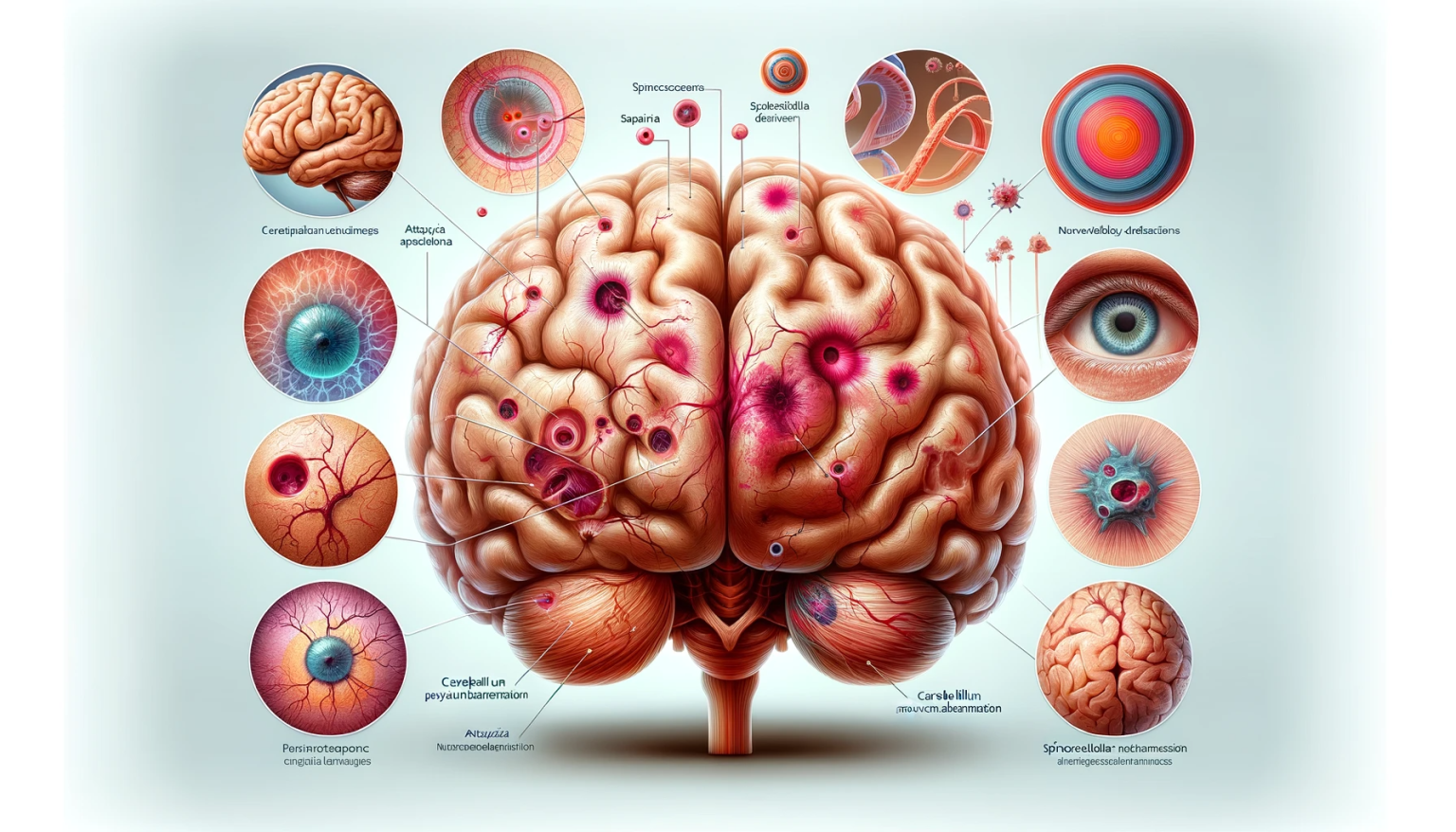
Clinical Manifestations:
- Diabetic Peripheral Neuropathy (DPN): The most common complication, presenting as distal symmetric polyneuropathy with sensory loss, pain, and sometimes motor involvement.
- Autonomic Neuropathy: Manifests as cardiovascular, gastrointestinal, genitourinary, and sudomotor dysfunction.
- Diabetic Amyotrophy: Characterized by proximal muscle weakness and atrophy, predominantly in the lower limbs.
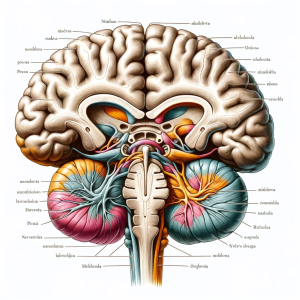
- Central Nervous System Effects: Cognitive impairment, an increased risk of cerebrovascular accidents, and mood disorders.
Diagnostic Approaches: Diagnosis of diabetic neurological complications involves:
- Clinical Assessment: Thorough neurological examination and symptom evaluation.
- Electrophysiological Studies: Nerve conduction studies and electromyography for peripheral neuropathies.
- Autonomic Testing: Assessing heart rate variability, sudomotor function, and other autonomic parameters.
- Imaging Studies: MRI or CT for central complications.
Management Strategies:
- Glycemic Control: Fundamental in preventing and slowing the progression of neurological complications.
- Pharmacotherapy: Pain management in DPN with antidepressants, anticonvulsants, and opioids.
- Physical Therapy and Rehabilitation: For motor deficits and muscle weakness.
- Multidisciplinary Approach: Addressing the multifaceted nature of diabetic neurological complications.
Conclusion: The neurological consequences of DM are diverse and significantly impact patient quality of life. Early recognition, rigorous glycemic control, and a comprehensive management approach are crucial for reducing morbidity.