Introduction
Graft-versus-host disease (GVHD) is a complex medical condition that occurs following allogeneic hematopoietic stem cell transplantation (HSCT). It arises when the donor immune cells, introduced into the recipient’s body, recognize the recipient’s tissues as foreign and initiate an immune response. This article aims to provide an in-depth understanding of GVHD, encompassing its pathophysiology, clinical manifestations, treatment options, and potential complications.
Pathophysiology of GVHD
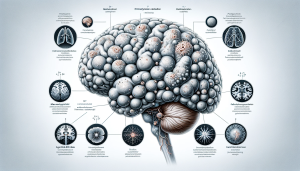
The pathogenesis of GVHD is fundamentally a multi-step process involving donor T-cell activation and proliferation. Initially, the conditioning regimens used in transplantation cause tissue damage, leading to the release of pro-inflammatory cytokines. These cytokines activate antigen-presenting cells (APCs), which then present host antigens to the donor T-cells. Subsequently, the activated T-cells proliferate and differentiate, orchestrating an immune attack against the host’s organs and tissues.
Clinical Manifestations
GVHD is classified into acute and chronic forms, each with distinct clinical features. Acute GVHD typically occurs within the first 100 days post-transplant and primarily affects the skin, liver, and gastrointestinal tract. Patients may present with a maculopapular rash, jaundice, and severe gastrointestinal symptoms like diarrhea. Chronic GVHD, on the other hand, can develop months to years after transplantation and often presents with more diverse symptoms, including skin changes, dry eyes and mouth, lung fibrosis, and musculoskeletal complications.
Diagnostic Criteria
Diagnosis of GVHD is predominantly clinical, supported by histopathological examination of biopsies from affected organs. The diagnostic criteria include the presence of typical symptoms post-HSCT, exclusion of other potential causes, and confirmatory biopsy findings. Recent advances in biomarkers are also contributing to more precise diagnosis and assessment of disease severity.
Treatment Strategies
The cornerstone of GVHD treatment is immunosuppression. First-line therapy for acute GVHD typically includes high-dose corticosteroids. In cases of steroid-refractory GVHD, second-line treatments like calcineurin inhibitors, anti-thymocyte globulin, or newer agents such as JAK inhibitors are considered. Chronic GVHD requires a more prolonged immunosuppressive regimen, often involving a combination of steroids, calcineurin inhibitors, and other agents like rituximab or ibrutinib.
Prevention and Prophylaxis
Prophylactic strategies are crucial in managing GVHD risk. These include careful donor selection, T-cell depletion techniques, and the use of prophylactic immunosuppressive drugs post-transplant. Additionally, advancements in the understanding of HLA matching and the development of reduced-intensity conditioning regimens have significantly contributed to reducing GVHD incidence.
Complications and Prognosis
GVHD significantly impacts the morbidity and mortality of HSCT recipients. Complications can range from infections due to prolonged immunosuppression to organ dysfunction. The prognosis of GVHD varies, with severity and response to initial treatment being key determinants. Chronic GVHD, in particular, can lead to long-term disability and impaired quality of life.
Conclusion
GVHD remains a challenging complication of allogeneic HSCT, with profound implications for patient outcomes. While advancements in prophylaxis and treatment have improved management, GVHD still requires a nuanced approach balancing graft-versus-tumor effects and host toxicity. Ongoing research and clinical trials continue to seek improved strategies for prevention, early detection, and treatment, with the ultimate goal of enhancing survival and quality of life for transplant recipients.