Abstract
Dentatorubral-Pallidoluysian Atrophy (DRPLA) is a rare, heritable neurodegenerative disorder characterized by ataxia, choreoathetosis, seizures, and cognitive deterioration. This review provides a comprehensive examination of the genetic etiology, neuropathological progression, clinical symptomatology, diagnostic methodologies, and current therapeutic modalities associated with DRPLA.
Introduction
DRPLA is a rare autosomal dominant disorder within the spectrum of polyglutamine diseases, caused by an abnormal CAG trinucleotide repeat expansion in the ATN1 gene. It manifests with a variety of progressive neurological symptoms that often begin in childhood or adolescence, though adult-onset forms exist. The disease is notable for its pleiotropic nature, displaying a range of clinical features that overlap with other neurodegenerative disorders, thereby complicating its diagnosis and management.
Genetic Origins
DRPLA is induced by an expanded CAG repeat in the ATN1 gene on chromosome 12p, which translates into a polyglutamine (polyQ) tract in the atrophin-1 protein. This expansion leads to neuronal toxicity through poorly understood mechanisms that include protein misfolding, aggregation, and interference with transcriptional regulation. The number of CAG repeats correlates with disease severity and inversely with the age of onset, a phenomenon observed across polyglutamine disorders.
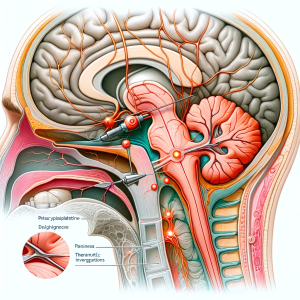
Neuropathological Progression
Neuropathologically, DRPLA is characterized by degeneration of the dentatorubral and pallidoluysian systems. Microscopic examination reveals neuronal loss, axonal swelling, and gliosis, with intranuclear inclusions present in the affected neurons. These inclusions contain the mutant atrophin-1 protein, suggesting a role in the pathogenesis. The disease progresses steadily, with increasing neuroanatomical involvement correlating with the expanding clinical syndrome.
Clinical Symptomatology
Clinically, DRPLA presents with a combination of cerebellar ataxia, involuntary movements such as chorea and dystonia, myoclonus, and epileptic seizures. Cognitive decline, ranging from mild impairment to severe dementia, is also a defining feature of the disorder. The juvenile form is often more aggressive, with rapid progression and a higher prevalence of seizures and myoclonus, while adult-onset cases may initially present with psychiatric symptoms or dementia.
Diagnostic Methodologies
The diagnosis of DRPLA relies on a combination of clinical assessment, family history, neuroimaging, and genetic testing. MRI of the brain typically shows atrophy of the cerebellum, brainstem, and basal ganglia. Genetic testing for CAG repeat expansion in the ATN1 gene confirms the diagnosis. Differential diagnosis includes Huntington’s disease, other spinocerebellar ataxias, and Wilson’s disease.
Clinical Management
Management of DRPLA is symptomatic and supportive. Pharmacological treatment may include antiepileptic drugs for seizures, medications to manage movement disorders, and cognitive enhancers for memory and concentration deficits. Physical and occupational therapies are important to maintain motor function and daily living activities. Genetic counseling is imperative for affected individuals and at-risk family members.
Conclusion
DRPLA is a debilitating genetic disorder with a significant impact on patients and families. While no cure exists, ongoing research aims to elucidate the mechanisms underlying neuronal degeneration and to develop targeted treatments. Multidisciplinary care is crucial to improve the quality of life for individuals with DRPLA.