Abstract
Alexander Disease (AD) is a rare, progressive neurodegenerative disorder, primarily affecting the white matter of the brain. This comprehensive review explores the genetic etiology, characteristic neuropathological features, clinical manifestations, diagnostic criteria, and current therapeutic approaches in AD.
Introduction
Alexander Disease, classified as a leukodystrophy, involves the degeneration and loss of myelin in the central nervous system. First described by W. Stewart Alexander in 1949, it is known for its distinctive neuropathological hallmark: the presence of Rosenthal fibers. AD predominantly affects infants and young children, but juvenile and adult-onset forms are also recognized.
Genetic Etiology
The disease is caused by dominant mutations in the GFAP gene, which encodes glial fibrillary acidic protein (GFAP), a key intermediate filament protein in astrocytes. These mutations lead to abnormal protein accumulation, contributing to the formation of Rosenthal fibers and subsequent myelin destruction. While most cases of AD are sporadic, familial cases have been reported, highlighting the role of genetic counseling in affected families.
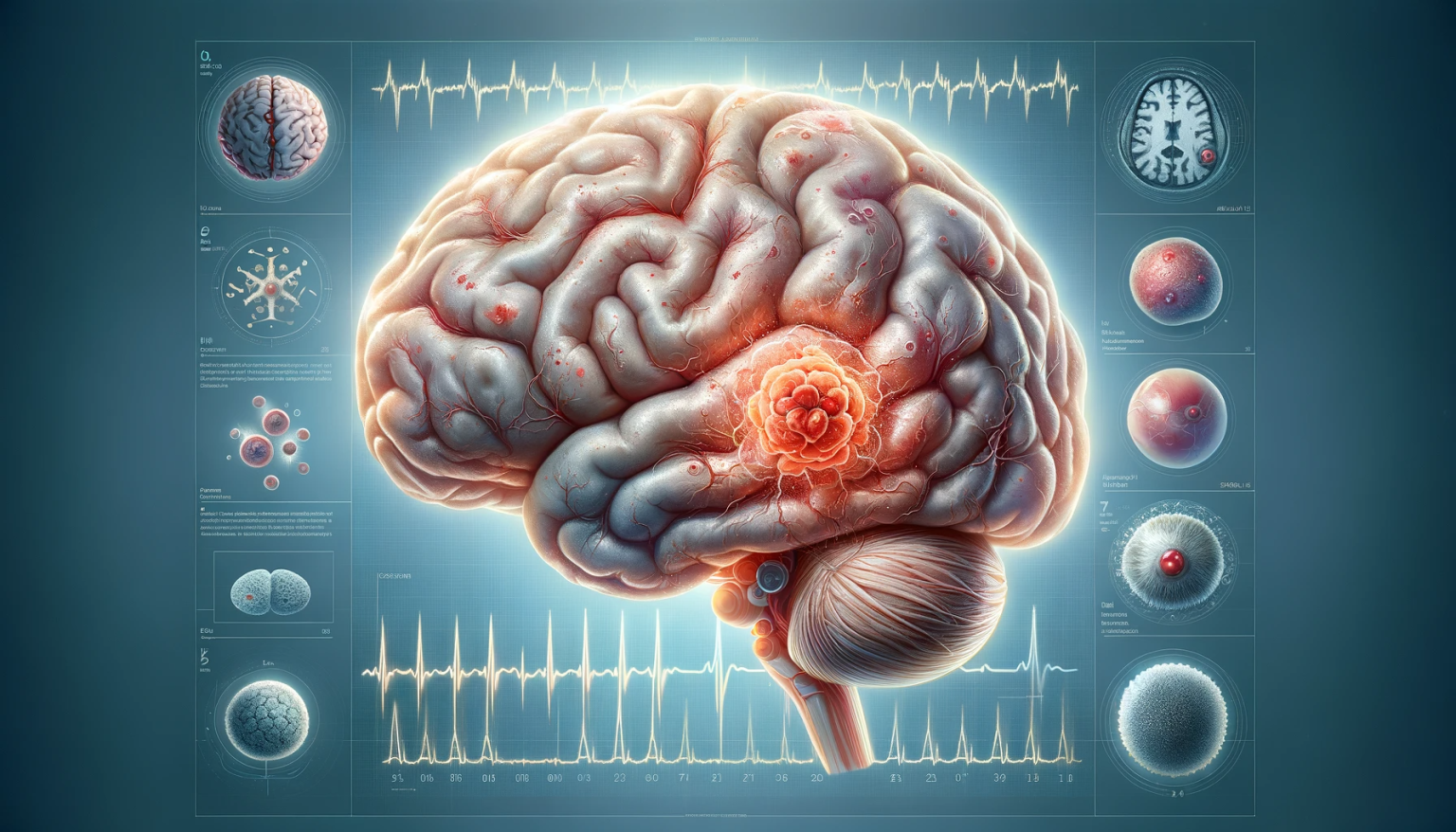
Neuropathological Features
AD is characterized by the widespread deposition of Rosenthal fibers within astrocytes, particularly in the subependymal, periventricular, and infratentorial regions. These fibers are eosinophilic, proteinaceous inclusions and are a pathognomonic feature of AD. Accompanying these changes are myelin loss, gliosis, and, in some cases, brain atrophy.
Clinical Presentation
The clinical presentation of AD varies with age of onset. Infantile AD typically presents with macrocephaly, developmental delay, seizures, and progressive psychomotor retardation. Juvenile and adult forms may have a more protracted course with bulbar and spinal cord symptoms, ataxia, and palatal myoclonus.
Diagnostic Approach
Diagnosis of AD is based on clinical presentation, imaging findings, and genetic testing. MRI typically shows frontal predominance white matter changes with contrast enhancement. Genetic testing confirms the diagnosis by identifying mutations in the GFAP gene. Differential diagnosis includes other leukodystrophies and neurodegenerative disorders.
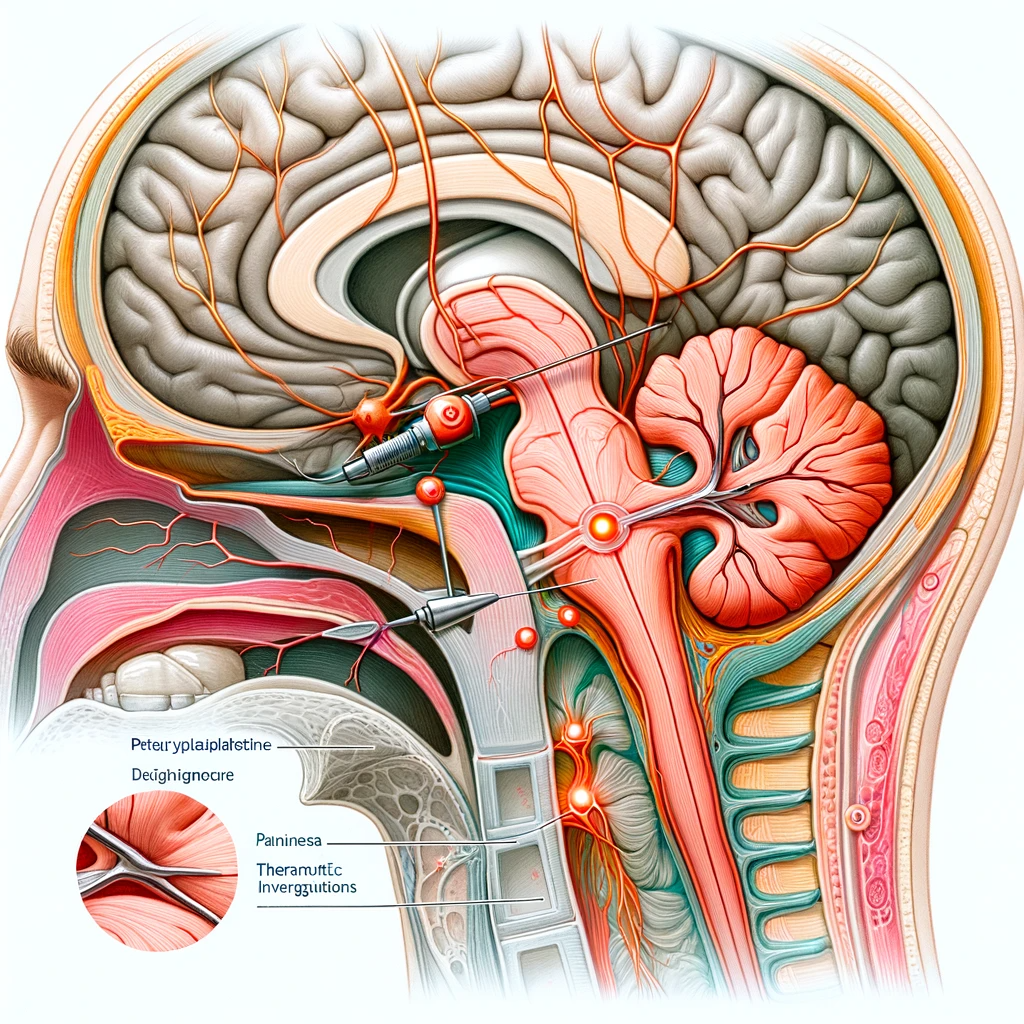
Therapeutic Management
Currently, no cure exists for AD, and treatment is largely symptomatic and supportive. Management involves a multidisciplinary team approach to address neurological symptoms, physical therapy to maintain mobility, and occupational therapy to support daily activities. Antiepileptic drugs are used for seizure control. Ongoing research into gene therapy and other novel treatments offers hope for future interventions.
Prognosis and Future Directions
The prognosis of AD varies, with the infantile form typically having a more severe course leading to early mortality. Advances in genetic research and understanding of the molecular pathology of AD are essential for developing targeted therapies.
Conclusion
Alexander Disease, with its distinct genetic and neuropathological features, presents unique challenges in neurology and genetics. Understanding its complex pathophysiology is crucial for developing effective therapeutic strategies and providing optimal care to affected individuals.