Introduction
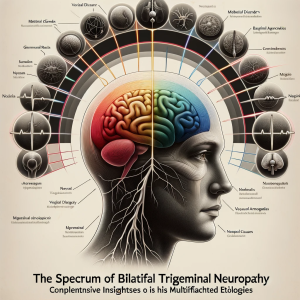
Bilateral trigeminal neuropathy is characterized by sensory and sometimes motor dysfunction in the distribution of the trigeminal nerve on both sides of the face. Though less common than unilateral presentations, its occurrence is associated with a diverse array of pathophysiological processes. This detailed exposition aims to expand upon the various etiological factors that can lead to bilateral trigeminal nerve impairment.The etiological landscape of bilateral trigeminal neuropathy is broad, encompassing infectious, systemic, neoplastic, and autoimmune conditions, alongside vascular, traumatic, and genetic factors.
Infectious agents
Infectious agents beyond Lyme disease and syphilis, such as herpes zoster, can cause bilateral manifestations if there is a reactivation within the trigeminal ganglia. HIV can also lead to bilateral trigeminal neuropathy through direct infection or secondary to opportunistic infections.
Autoimmune disorders
Autoimmune disorders, including Sjögren’s syndrome and systemic lupus erythematosus, have been implicated in bilateral trigeminal neuropathy due to their systemic inflammatory effects, which can lead to nerve damage. Similarly, sarcoidosis can involve the cranial nerves bilaterally through granulomatous infiltration.
Aberrations in blood vessels
Vascular anomalies, such as aneurysms or arteriovenous malformations, can compress the trigeminal nerve roots bilaterally, particularly in cases where there is a significant vascular loop or aberrant vessels.
Trauma
Trauma to the skull base or iatrogenic injury during surgical procedures may result in bilateral damage to the trigeminal nerve. Genetic disorders like familial dysautonomia (Riley-Day syndrome) can present with bilateral trigeminal impairment due to the inherited neuropathic process. Environmental and occupational factors, such as exposure to neurotoxic chemicals or heavy metals, have been associated with peripheral neuropathies, including the trigeminal nerve, in a bilateral distribution.
Disorders of metabolism
Metabolic disorders, notably diabetes mellitus, can lead to a symmetrical neuropathy, including the cranial nerves. Furthermore, vitamin deficiencies, particularly B12, can affect nerve function bilaterally due to the generalized nature of the neuropathy associated with such deficiencies.
Oncogenic origins
Neoplastic causes extend to lymphomas and bilateral schwannomas, which, although rare, can cause bilateral trigeminal nerve involvement due to their growth patterns or multifocal presentations.
Conclusion
The diagnostic conundrum of bilateral trigeminal neuropathy necessitates a sophisticated and nuanced approach. Clinicians must rely on a comprehensive clinical assessment, including a meticulous patient history and a thorough neurological examination. The blink reflex test emerges as a significant
diagnostic tool within this context. Abnormalities in R1 latency, either protracted (exceeding 20 milliseconds) or abbreviated (below 12 milliseconds), can serve as indicators of pathological changes within the trigeminal nerve pathways.
Such deviations from the normative latency values may herald the presence of neuropathic processes and should prompt further investigative measures to confirm the diagnosis of trigeminal neuropathy. This method underscores the importance of integrating neurophysiological testing in the diagnostic algorithm to facilitate the detection of trigeminal nerve dysfunction and guide subsequent management plans for the condition.